Beam hardening
"soft" = low energy; "hard" = high energy
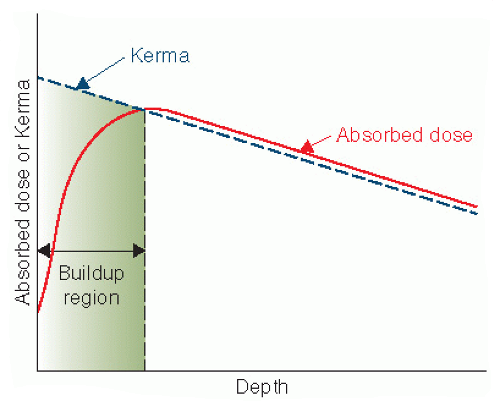
As the beam with a spectrum of energies passes through the patient, low energy photons are absorbed more easily, leaving more high energy in the spectrum.
This means that tissue near the surface gets more attenuation, and deep tissue gets less.
The consequences are: (a) most damage near the skin (which is also sensitive to radiation damage); and (b) poorer imaging of deep tissue.
This is like an "aerial perspective" effect, but with a different mechanism:

Noise
"Noise" is variance in the measured signal with respect to the true signal.
Usually modelled with a zero-mean Gaussian, unless there's bias.
"SNR" is the signal-to-noise ratio. This is ${P_\textrm{signal} \over P_\textrm{noise}} = ({A_\textrm{signal} \over A_\textrm{noise}})^2$ where $P$ is power and $A$ is amplitude.
SNR is proportional to ${1 \over \sqrt{N}}$, for $N$ = the number of photons, so quadrupling the number of photons will only halve the noise (i.e. the variance).
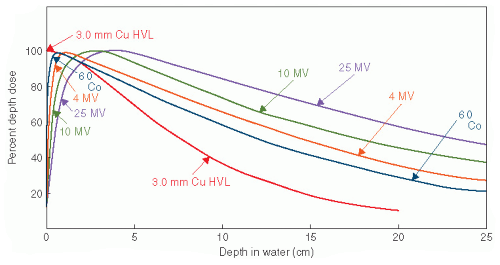
Consequences: Image noise can be reduced with more photons, which can be achieved with more photon flow (more mA) or with a higher xray energy (higher keV), since the number of photons is also proportional to $(kV)^3$. But higher keV photons don't interact as much with tissue, so don't help too much.
On the X-ray machine, three things can be adjusted to determine dose:
- energy (machine's kV)
- quantity (machines mA)
- exposure duration (time)
Blur
Comes from non-point-source of xrays.
Comes from patient motion.
Contrast
"Contrast" is the difference in appearance of different tissues in the xray image.
Different materials have different absorption profiles:
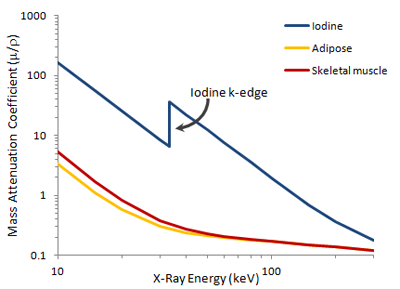
The "mass attenuation coefficient" above, ${\mu \over \rho}$, has the linear attenuation coefficient, $\mu$ in cm$^{-1}$, from the Beer-Lambert law and has the material density, $\rho$ in g/cm$^3$.
There is a greater attenuation difference between materials at low energies.
Consequence: Image contrast can be improved with lower kV. However, lower-energy photons are more easily stopped by tissue, so this is at the cost of a higher dose.
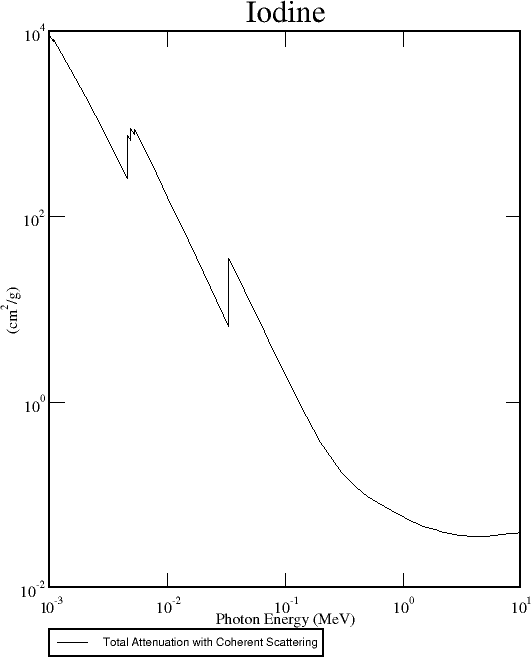
The "k-edge" is the energy required to dislodge an innermost (k orbital) electron from an atom. This is also the most likely energy at which the photoelectric effect (i.e. absorption) occurs.
Other edges exist at lower energies: The leftmost edge below is the "l-edge" for Iodine. If the x-ray photon energy is greater than the binding energy of the k-orbital electrons, the k-orbital electrons are more likely to be dislodged.
Iodine and barium have k-edges at 33 keV and 37 keV, respectively, which are in middle of the typical xray spectrum.
Consequence: Iodine and barium make good constrast agents.
Some different tissues with different absorption spectra:
 [ radiologykey.com ]
[ radiologykey.com ]
 [ radiologykey.com ]
[ radiologykey.com ]